MoviPrep Cleansing Procedure for Colonoscopy
Movi Prep for Colonoscopy
PAUL E. SAVOCA, MD, FACS, FASCRS
PLEASE READ THE FOLLOWING INSTRUCTIONS CAREFULLY BEFORE YOUR PROCEDURE:
All PATIENTS MUST FOLLOW A CLEAR LIQUID DIET ONLY ALL DAY THE DAY PRIOR TO COLONOSCOPY.
DO NOT EAT OR DRINK ANYTHING OTHER THAN YOUR PREP AFTER MIDNIGHT THE NIGHT BEFORE
- DO NOT eat foods containing seeds for five days prior to your procedure such as sesame or poppy seeds, strawberries, black pepper, corn or tomato skins. If by chance you have eaten these products, you should still proceed with your preparation.
- Prescribed medications for heart disease, high blood pressure and asthma may be taken prior to your procedure, unless otherwise instructed. All other medications, including diabetic medications, should be brought along with you to be taken after your procedure.
- DO NOT take aspirin or aspirin-type products such as Ibuprofen, Advil, Aleve, Nuprin, Motrin, Naprosyn, etc. for at least one week prior to procedure. Please do not take herbal remedies or supplements for at least one week prior to your exam. You may take Tylenol.
- After your colonoscopy, if you had a biopsy or polyp removed: Please stop Plavix 7 days prior to your procedure, or Coumadin 4 days prior. Please consult the physician who prescribed the medication to make them aware.
- Please advise the physician if you have a prosthetic heart valve, a serious heart murmur, or if you have had any cardiac procedures in the last year.
- On the day of your colonoscopy you will receive intravenous sedation. These medications will impair your driving ability. You must arrange for someone to take you home after your procedure. The driver must remain in the facility throughout your procedure and recovery. You may not drive until the next day.
- You will receive written diet instructions after your colonoscopy.
- This packet contains the Movi-prep. If you are unable to complete the prep, please call the Doctor’s office and speak with a staff member. After hours, the Physician on call will contact you.
Movi Prep for Colonoscopy
Patient Instructions – Split – Dose Regimen
The MoviPrep carton contains 4 pouched and a disposable container for mixing. You must complete the entire prep to ensure the most effective cleansing.
The evening before your colonoscopy beginning at: 6pm
Step 1: Mix First Dose
- Empty 1 Pouch A and 1 Pouch B into the disposable container
- Add lukewarm drinking water to the top line of the container and mix until dissolved. If preferred, mix solution ahead of time and refrigerate prior to drinking. The solution should be used within 24 hours.
Step 2: Drink First Dose
- The MoviPrep container is divided by 4 marks. Every 15 minutes, drink the solution down to the next mark (approximately 8 oz), until the full liter is consumed
- Drink 16 oz of the clear liquid of your choice. This is a necessary step to ensure adequate hydration and an effective prep.
Step 3: Mix Second Dose
- Empty 1 Pouch A and 1 Pouch B into the disposable container
- Add lukewarm drinking water to the top line of the container and stir well If preferred, mix solution ahead of time and refrigerate prior to drinking. The reconstituted solution should be used within 24 hours.
Step 4: Drink the second dose the morning of your colonoscopy. You must COMPLETE drinking it four hours prior to leaving for your procedure.
- The MoviPrep container is divided by 4 marks. Every 15 minutes, drink the solution down to the next mark (approximately 8 oz), until the full liter is consumed.
- Do not drink or eat anything after completing the last does of your MoviPrep.
This colonoscopy prep causes the body to lose a significant amount of fluid and can result in dehydration. It’s important that you prepare your body by drinking extra clear liquids before the prep and remaining hydrated by drinking all required clear liquids during the prep. Also, replenish your system by drinking clear liquids after returning home from your colonoscopy.
If you have any questions, please call our office at 631-862-3600
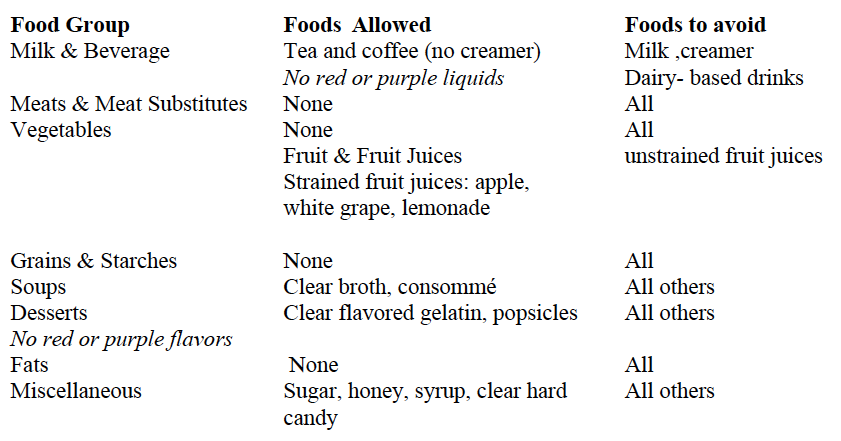
CLEAR LIQUID DIET
This diet provides fluids that leave little residue and are easily absorbed with minimal digestive activity. This diet is inadequate in all essential nutrients and is recommended only if clear liquids are temporarily needed.
No red or purple liquids should be consumed!