Screening for Colorectal Cancer
Screening & Surveillance for Colorectal Cancer
What is the risk of colorectal cancer?
Colorectal cancer is the second most common cancer in the United States. The average person’s lifetime risk of developing it is about one chance in 20. The risk is increased if there is a family history of colorectal polyps or cancer, and is still higher if there is a personal history of breast, uterine or ovarian cancer. Risk is also higher for people with a history of extensive inflammatory bowel disease, such as ulcerative or Crohn’s colitis.
What is screening and surveillance?
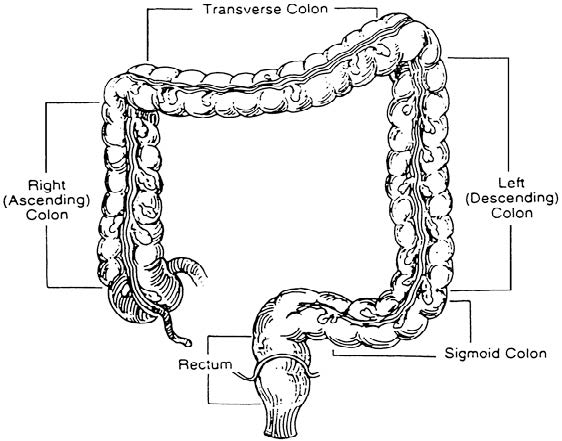
Many polyps and cancers of the colon and rectum do not produce symptoms until they become fairly large. Screening involves one or more tests performed to identify whether a person with no symptoms has a disease or condition that may lead to colon or rectal cancer. The goal is to identify the potential for disease or the condition early when it is easier to prevent or cure. Surveillance involves testing people who have previously had colorectal cancer or are at increased risk. Because their chance of having cancer is higher, more extensive or more frequent tests are recommended.
Later in the brochure, the tests and risk groups are defined. Also, your physician can further explain the tests and their value to you.
Why should testing be undertaken?
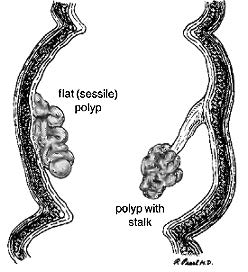
Colorectal cancer is known as a “silent” disease, because many people do not develop symptoms, such as bleeding or abdominal pain until the cancer is difficult to cure. In fact, the possibility of curing patients after symptoms develop is only about 50%. On the other hand, if colorectal cancer is found and treated at an early stage, before symptoms develop, the opportunity to cure is 80% or better. Most colon cancers start as non cancerous growths called polyps. If the polyps are removed, then the cancer may be prevented. Major surgery can usually be avoided.
What screening tests should be done?
The simplest screening test for colon and rectal cancer is testing of the stool to detect tiny amounts of invisible blood; this is called fecal occult blood testing.This test has been available for many years, is inexpensive and very simple. Unfortunately, it only detects cancer or polyps which are bleeding at the time of the test. Only about 50% of cancers and 10% of polyps bleed enough to be detected by this test. Therefore, further screening is necessary for accurate detection of cancers and polyps.
Flexible sigmoidoscopy is a test which allows the physician to look directly at the lining of the colon and rectum. During this test, which is performed in the physician’s office, the lining of the lower one-third of the colon and rectum can usually be seen. This is the portion of the lower intestine which accounts for most polyps and cancers. When flexible sigmoidoscopy is combined with testing the stool for hidden blood, many cancers and polyps can be detected.
When a polyp or cancer is detected by flexible sigmoidoscopy, or if a person is at high risk to develop colon and rectal cancer, colonoscopy provides a safe, effective means of visually examining the full lining of the colon and rectum. Colonoscopy is used to diagnose colon and rectal problems and to perform biopsies and remove colon polyps. Most colonoscopies are done on an outpatient basis with minimal inconvenience and discomfort.
A barium enema or x-ray of the colon is almost as good as colonoscopy in detecting large tumors, but it is not as accurate for small tumors or polyps. The combination of barium enema and sigmoidoscopy is better than either test alone, but not as good as colonoscopy.
When and how often should testing be done?
For people who have none of the risks described earlier, digital rectal examination and testing of the stool for hidden blood are recommended annually beginning at age 40. Flexible sigmoidoscopy is recommended every 5 years at age 50 or older. A double contrast barium enema every 5 to 10 years, and colonoscopy every 10 years are acceptable alternatives.
Surveillance is recommended for people in the following high-risk groups:
- People who have had any pre-cancerous polyps found and removed should have colonoscopy one to three years after the first examination. Double-contrast barium enema is an alternative to colonoscopy but does not allow removal of polyps.
- People with a close relative, such as sibling, parent or child who has had colorectal cancer or a pre-cancerous polyp should have the same screening as people of average risk, but it should begin at age 40 or 5 years before the age at which the youngest was diagnosed.
- People with a family history of colorectal cancer in several close relatives and several generations, especially cancers occurring at a young age, should receive genetic counseling and consider genetic testing for a condition called hereditary nonpolyposis colorectal cancer. People with this family medical history should have an examination of the entire colon preferably colonoscopy every two years starting between the age of 20 and 30, and every year after age 40.
- People with a family history of an inherited disease called familial adenomatous polyposis (FAP) should receive counseling and consider genetic testing to see if they are carriers for the gene that causes the disease. People with this gene or whose tests are inconclusive should have a flexible sigmoidoscopy annually beginning at puberty to see if they are expressing the gene. If polyposis is present, they should discuss with their physician the need for total colectomy, which involves removing all the colon and rectum.
- People with a personal history of colorectal cancer should have a complete examination of the colon within one year after the cancer is initially detected and surgically removed. If this exam is normal, they should have a follow-up exam within three years. Examinations to evaluate the entire colon include colonoscopy or flexible sigmoidoscopy with adouble-contrast barium enema.
- People with a history of extensive inflammatory bowel disease for 8 or more years should consider having a colonoscopy examination of their colon conducted every one to two years.
- Women with a personal history of breast or female genital cancer (ovary or uterine) have a 15%lifetime risk (1 in 6) of developing colon cancer. They should undergo colonoscopy every 5 years, beginning at age 40.
Who does the screening and surveillance?
The simpler tests such as digital rectal examination, fecal occult blood testing, or flexible sigmoidoscopy may be performed by your primary care physician or your surgeon. They can also arrange for colonoscopy to be performed by a specially trained physician, such as a colon and rectal surgeon.