General Colonoscopy Information
Colonoscopy
What is colonoscopy?
Colonoscopy is a safe, effective method of examining the full lining of the colon and rectum, using a long, flexible, tubular instrument. It is used to diagnose colon and rectum problems and to perform biopsies and remove colon polyps. Most colonoscopies are done on an outpatient basis with minimal inconvenience and discomfort.
Who should have a colonoscopy?
Colonoscopy is routinely recommended to adults 50 years of age or older as part of a colorectal cancer screening program. Patients with a family history of colon or rectal cancer may have their colonoscopy at age 40. Your physician may also recommend a colonoscopy exam if you have change in bowel habit or bleeding, indicating a possible problem in the colon or rectum.
A colonoscopy may be necessary to:
• Check unexplained abdominal symptoms
• Check inflammatory bowel disease (colitis)
• Verify findings of polyps or tumors located with a barium enema exam
• Examine patients who test positive for blood in the stool
• Monitor patients with a personal or family history of colon polyps or cancer.
How is colonoscopy performed?
The bowel must first be thoroughly cleared of all residue before a colonoscopy. This is done one to two days before the exam with a preparation prescribed by your physician.
Many patients receive intravenous sedation, or “twilight sleep” for this procedure. The colonoscope is inserted into the rectum and is advanced to the portion of the colon where the small intestine joins the colon. During a complete examination of the bowel, your physician will remove polyps or take biopsies as necessary.
The entire procedure usually takes less than an hour. Following the colonoscopy, there may be slight discomfort, which quickly improves with the expelling of gas. Most patients can resume their regular diet and activities the same day.
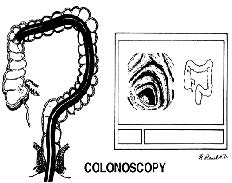
Left: Flexible fiberoptic colonoscope in place examining the lining of the colon.
Right: Image of the portion of the colon being examined on the television monitor.
What are the benefits of colonoscopy?
Colonoscopy is more accurate than an x-ray exam of the colon to detect polyps or early cancer. With colonoscopy, it is now possible to detect and remove most polyps without abdominal surgery. Removing polyps is an important step in the prevention of colon cancer.
What are the risks of colonoscopy?
Colonoscopy is a very safe procedure with complications occurring in less than 1% of patients. These risks include bleeding, a tear in the intestine, risks of anesthesia and failure to detect a polyp.
Colonoscopy
A colonoscopy is an exam to evaluate your entire colon. In this exam, your colon is cleansed. A long fiberoptic tube is inserted through your rectum and into your colon. The fiberoptic scope (endoscope) is a long bundle of enclosed and very flexible fibers. These fibers transmit light to the area examined and send images from that area to your caregiver. Discomfort is usually minimal. You may be given a drug to help you sleep (sedative) during or prior to the procedure. This exam helps to detect lumps (tumors), polyps, inflammation, and areas of bleeding. Your caregiver may also take a small piece of tissue (biopsy) that will be examined under a microscope.
BEFORE THE PROCEDURE
A clear liquid diet may be required for 2 days before the exam.
-Liquid injections (enemas) or laxatives may be required.
-A large amount of electrolyte solution may be given to you to drink over a short period of time. This solution is used to clean out your colon.
-You should be present 1 hour prior to your procedure or as directed by your caregiver.
-Check in at the admissions desk to fill out necessary forms if not preregistered. There will be consent forms to sign prior to the procedure. If accompanied by friends or family, there is a waiting area for them while you are having your procedure.
LET YOUR CAREGIVER KNOW ABOUT:
-Allergies to food or medicine.
-Medicines taken, including vitamins, herbs, eyedrops, over-the-counter medicines, and creams.
-Use of steroids (by mouth or creams).
-Previous problems with anesthetics or numbing medicines.
-History of bleeding problems or blood clots.
-Previous surgery.
-Other health problems, including diabetes and kidney problems.
-Possibility of pregnancy, if this applies.
AFTER THE PROCEDURE
-If you received a sedative and/or pain medicine, you will need to arrange for someone to drive you home.
-Occasionally, there is a little blood passed with the first bowel movement. DO NOT be concerned.
HOME CARE INSTRUCTIONS
-It is not unusual to pass moderate amounts of gas and experience mild abdominal cramping following the procedure. This is due to air being used to inflate your colon during the exam. Walking or a warm pack on your belly (abdomen) may help.
-You may resume all normal meals and activities after sedatives and medicines have worn off.
-Only take over-the-counter or prescription medicines for pain, discomfort, or fever as directed by your caregiver. DO NOT use aspirin or blood thinners if a biopsy was taken. Consult your caregiver for medicine usage if biopsies were taken.
FINDING OUT THE RESULTS OF YOUR TEST
Not all test results are available during your visit. If your test results are not back during the visit, make an appointment with your caregiver to find out the results. Do not assume everything is normal if you have not heard from your caregiver or the medical facility. It is important for you to follow up on all of your test results.
SEEK IMMEDIATE MEDICAL CARE IF:
-You have an oral temperature above 102° F (38.9° C), not controlled by medicine.
-You pass large blood clots or fill a toilet with blood following the procedure. This may also occur 10 to 14 days following the procedure. This is more likely if a biopsy was taken.
-You develop abdominal pain that keeps getting worse and cannot be relieved with medicine.
Document Released: 04/07/2004 Document Re-Released: 03/14/2011
ExitCare® Patient Information ©2011 ExitCare, LLC.