Colorectal Cancer
Colorectal cancer is the second most common cancer in the United States, striking 140,000 people annually and causing 60,000 deaths. That’s a staggering figure when you consider the disease is potentially curable if diagnosed in the early stages.
Who is at risk?
Though colorectal cancer may occur at any age, more than 90% of the patients are over age 40, at which point the risk doubles every ten years. In addition to age, other high risk factors include a family history of colorectal cancer and polyps and a personal history of ulcerative colitis, colon polyps or cancer of other organs, especially of the breast or uterus.
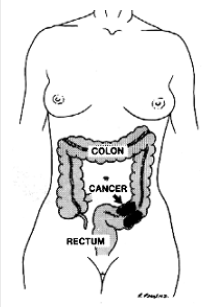
How does it start?
It is generally agreed that nearly all colon and rectal cancer begins in benign polyps. These pre-malignant growths occur on the bowel wall and may eventually increase in size and become cancer. Removal of benign polyps is one aspect of preventive medicine that really works!
What are the symptoms?
The most common symptoms are rectal bleeding and changes in bowel habits, such as constipation or diarrhea. (These symptoms are also common in other diseases so it is important you receive a thorough examination should you experience them.) Abdominal pain and weight loss are usually late symptoms indicating possible extensive disease.
Unfortunately, many polyps and early cancers fail to produce symptoms. Therefore, it is important that your routine physical includes colorectal cancer detection procedures once you reach age 50. There are several methods for detection of colorectal cancer.
These include digital rectal examination, a chemical test of the stool for blood, flexible sigmoidoscopy and colonoscopy (lighted tubular instruments used to inspect the lower bowel) and barium enema. Be sure to discuss these options with your surgeon to determine which procedure is best for you. Individuals who have a first-degree relative (parent or sibling) with colon cancer or polyps should start their colon cancer screening at the age of 40.
How is colorectal cancer treated?
Colorectal cancer requires surgery in nearly all cases for complete cure. Radiation and chemotherapy are sometimes used in addition to surgery. Between 80-90% are restored to normal health if the cancer is detected and treated in the earliest stages. The cure rate drops to 50% or less when diagnosed in the later stages. Thanks to modern technology, less than 5% of all colorectal cancer patients require a colostomy, the surgical construction of an artificial excretory opening from the colon.
Can colon cancer be prevented?
Colon cancer is preventable. The most important step towards preventing colon cancer is getting a screening test. Any abnormal screening test should be followed by a colonoscopy. Some individuals prefer to start with colonoscopy as a screening test.
Colonoscopy provides a detailed examination of the bowel. Polyps can be identified and can often be removed during colonoscopy.
Though not definitely proven, there is some evidence that diet may play a significant role in preventing colorectal cancer. As far as we know, a high fiber, low fat diet is the only dietary measure that might help prevent colorectal cancer.
Finally, pay attention to changes in your bowel habits. Any new changes such as persistent constipation, diarrhea, or blood in the stool should be discussed with your physician.
Can hemorrhoids lead to colon cancer?
No, but hemorrhoids may produce symptoms similar to colon polyps or cancer. Should you experience these symptoms, you should have them examined and evaluated by a physician, preferably by a colon and rectal surgeon. Colorectal Cancer Surgery-Follow Up Evaluation
Colorectal Cancer Surgery-Follow Up Evaluation
Why should there be a postoperative follow-up program?
Surgery is the most effective treatment for colorectal cancer. Even when all visible cancer has been removed, it is possible for cancer cells to be present in other areas of the body. These cancer deposits, when very small, are undetectable at the time of surgery, but they can begin to grow at a later time. The chance of recurrence depends on the characteristics of the original cancer and the effectiveness of chemotherapy, if needed, or other follow up treatment. Patients with recurrent cancers – if diagnosed early – may benefit, or be cured, by further surgery or other treatment.
Another good reason for postoperative follow up is to look for new colon or rectal polyps. Approximately one in five patients who has had colon cancer will develop a new polyp at a later time in life. It is important to detect and remove these polyps before they become cancerous.
How long will my follow-up program last?
Most recurrent cancers are detected within the first two years after surgery. Therefore, follow up is most frequent during this period of time. After five years, nearly all cancers that are going to recur will have done so. Follow up after five years is primarily to detect new polyps, and can, therefore, be less frequent but advisable for life.
What might I expect at my follow-up visit?
Your doctor will examine you approximately every two or three months for the first two years, and discuss your progress. A CEA blood test can be done, as a method of trying to detect recurrence of cancer. Because this test is not totally reliable, other follow up examinations may be advised. These examinations may include flexible sigmoidoscopy (an examination of the rectum and lower colon with a flexible, lighted instrument), colonoscopy (examination of the entire colon with a long flexible instrument), chest x-rays, and sometimes CT scans or ultrasound tests.
What about my family?
Close relatives of patients with colon and rectal cancer (parents, brothers, sisters, children) are at increased risk for the disease. Because of this, periodic examination of the lining of the colon, using a colonoscope to detect small polyps, is advised. If polyps are promptly detected and removed, cancers cannot develop. Other factors which increase the risk of developing polyps or cancer include cancer occurring at an early age, and a personal history of breast or female genital cancer.